High protein diets have become popular in the athletic and weight loss spheres in recent decades. But is loading-up on protein effective or safe over the long term?
According to recent studies, the answer is a firm “no” on both counts.
A 2022 meta-analysis, published in the Journal of Cachexia, Sarcopenia and Muscle, found there is no benefit to consuming more protein than the recommended daily allowance provided by most governments and the National Academy of Medicine.
Another 2022 study found extra protein intake only worked when it was coupled with vigorous exercise. Moreover, even for muscle-building athletes, there is a dose response where that benefit quickly tapers off—and the upper limit was nowhere near as high as most people thought.
Researchers involved in these studies point out that while extra protein can be beneficial in certain circumstances—such as for pregnant women or extreme athletes—the extra protein required is much smaller than people realize. The body still needs a lot more (healthy) carbohydrates than protein.
Health risks
In addition to the question of effectiveness is the health risks that come with excess protein. While there is much debate on the issue, decades of studies have drawn attention to increased risk of gout, cancer, heart disease and kidney conditions. Even over the short-term, protein can cause issues such as constipation due to lack of fiber.
Now a new study, published in February 2024, has corroborated that excess protein in the diet is bad for the heart, and has even pinpointed the upper safety limit.
The research, conducted by University of Pittsburgh School of Medicine researchers, revealed that a diet exceeding 22 percent of daily caloric intake from protein drastically increased the risk of atherosclerosis.
Well-known natural health advocate Dr. Joseph Mercola is perhaps the highest-profile health advocate who has changed his view on high protein diets.
In his article Basic Tips for Optimal Health on February 29, 2024, Dr. Mercola remarked:
“One of the foundational concepts of health that I’ve radically revised my thinking on is the idea that a low-carb diet is the best way to optimize your metabolic health. That was misguided, because when glucose is absent, your body releases cortisol to produce endogenous glucose. Cortisol sacrifices lean muscle mass, bone and your brain to make glucose, which triggers inflammation and impairs your immune function.”
The current study demonstrating higher risk of atherosclerosis when protein consumption is 22% and higher in the diet is just one more reason that experts of this caliber will continue to change their view.
Atherosclerosis is a condition characterized by the hardening and narrowing of arteries due to plaque buildup.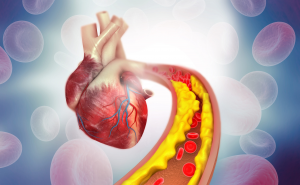
According to the findings, the research team conducted a comprehensive investigation combining human trials with animal and cellular studies.
Their research revealed complex molecular mechanisms whereby high protein consumption lead to increased activation of immune cells—the very immune cells that have been implicated in the formation of atherosclerotic plaque, and ultimately heart disease.
Part of the research included a series of experiments to explore how amino acids from protein influence disease processes at the molecular level. The experiments demonstrated that high dietary protein intake disrupted the normal function of these cells, leading to the accumulation of cellular debris within the arterial walls.
“Our study shows that dialing up your protein intake in pursuit of better metabolic health is not a panacea. You could be doing real damage to your arteries,” noted senior study author Dr. Babak Razani, professor of cardiology at the University of Pittsburgh, in a university release. “Our hope is that this research starts a conversation about ways of modifying diets in a precise manner that can influence body function at a molecular level and dampen disease risks.”
Based on the findings of the study, those who still insist on high protein diet may want to at least reduce the amount that is derived from animal sources.
According to the researchers, a critical aspect of the study was the implication of leucine, an amino acid predominantly found in animal-based foods such as beef, eggs, and milk. According to the researchers, leucine was a “key player” in promoting the pathways associated with atherosclerosis.
The researchers readily admit that the context for their research was the growing popularity of high-protein diets “driven by widespread beliefs in their health benefits, including muscle maintenance and weight loss.”
However, according to the researchers, while protein is a critical component in the human diet, high amounts of protein is detrimental rather than beneficial: “This study challenges the notion that more protein is invariably better, suggesting that over-reliance on protein, especially from animal sources, may have unintended health consequences.”
protein is detrimental rather than beneficial: “This study challenges the notion that more protein is invariably better, suggesting that over-reliance on protein, especially from animal sources, may have unintended health consequences.”
ProActive Wellness & Injury Centre has promoted a 60-20-20 diet ratio since the 1990s (60% carbs, 20% protein and 20% fat).
Obviously, this amount can be adjusted slightly depending on a person’s age, certain health conditions and athletic prowess; however, as a basic starting point for the average person, this guideline has proven effective for tens of thousands of people during the past 30 years.
The proper amount of protein ingested regularly will go a long way in promoting “the best performance of your life!”
God bless,
DrB
Sources: Nature Metabolism; Journal of Cachexia, Sarcopenia and Muscle.